Health Insurance Payout Ratio (également appelé Medical Loss Ratio ou MLR) désigne le pourcentage des primes de santé qu’un assureur consacre réellement aux soins médicaux et à l’amélioration de la qualité, par opposition aux frais d’administration ou au bénéfice. Comprendre ce ratio est essentiel pour les consommateurs américains : il permet d’évaluer si leur prime sert principalement à financer les prestations de santé. Depuis l’Affordable Care Act (ACA), la loi impose un seuil minimal — 80 % pour le marché individuel et les petits groupes, 85 % pour les grands groupes — et exige le remboursement des assurés lorsque ce seuil n’est pas atteint. Cet article explique de façon pédagogique comment fonctionne le Health Insurance Payout Ratio, pourquoi il influence le prix des primes et ce que disent les statistiques fédérales et étatiques les plus récentes.
On This Page
Essential Overview
Health insurance payout ratios measure how much premium revenue insurers spend on medical claims versus administrative costs, with federal regulations requiring most insurers to spend at least 80-85% on healthcare services.
What is a good claim settlement ratio for health insurance?
A strong health insurance claim settlement ratio typically ranges from 95% to 98%, indicating the insurer approves and pays the vast majority of legitimate claims submitted by policyholders. This metric directly reflects an insurer’s commitment to honoring coverage obligations and protecting members’ financial interests.
PRO TIP Look for insurers with settlement ratios above 96% and declining denial rates over multiple years to identify companies prioritizing member care over profit maximization.
The claim settlement ratio represents the percentage of submitted claims that receive full or partial payment from the insurance company. Unlike simple approval rates, this metric accounts for the actual dollar value of claims processed, providing a more accurate picture of insurer reliability during medical emergencies.
| Settlement Ratio Range | Insurer Performance | Consumer Impact |
|---|---|---|
| 97-98% | Excellent | Minimal claim denials |
| 95-96% | Good | Occasional disputes |
| 92-94% | Average | Moderate denial risk |
| Below 92% | Concerning | Higher denial likelihood |
Key factors influencing settlement ratios include:
- Prior authorization requirements and efficiency
- Network adequacy and provider relationships
- Claims processing technology and staff training
- Medical necessity review procedures
- Appeals and grievance resolution effectiveness
State insurance departments track settlement ratios through annual reports, with federal health insurance oversight showing significant variation between insurers. Companies maintaining consistently high ratios demonstrate operational excellence and member-focused policies.
IMPORTANT NOTE Settlement ratios below 95% may indicate aggressive denial practices, inadequate network coverage, or poor claims processing systems that could delay necessary medical care.
Consumer protection improves when insurers maintain transparent claims procedures, reasonable denial rates, and efficient appeals processes. Members benefit from understanding these metrics before selecting coverage, particularly for chronic conditions requiring ongoing medical management through comprehensive health insurance plans.
What is the 80 20 rule for health insurance?
The 80/20 rule, formally known as the Medical Loss Ratio (MLR) requirement, mandates that health insurers spend at least 80% of premium revenue on medical care and quality improvement activities, limiting administrative costs and profits to 20% maximum.
This federal regulation applies to individual and small group markets, while large group plans face an 85% MLR requirement. The rule ensures premium dollars directly benefit policyholders through healthcare services rather than excessive administrative overhead or shareholder profits.
Breakdown of the 80/20 allocation:
Medical Care (80% minimum):
- Direct payments to healthcare providers
- Prescription drug costs
- Medical equipment and supplies
- Quality improvement programs
- Care coordination initiatives
Administrative Costs (20% maximum):
- Claims processing operations
- Customer service departments
- Marketing and sales expenses
- Executive compensation
- Shareholder dividends and profits
| Market Segment | MLR Requirement | Rebate Threshold |
|---|---|---|
| Individual Plans | 80% | Below 80% |
| Small Group | 80% | Below 80% |
| Large Group | 85% | Below 85% |
The Centers for Medicare & Medicaid Services shows that insurers failing to meet these thresholds must issue rebates to policyholders, with over $2.7 billion in rebates distributed in recent years.
Consumer benefits of MLR requirements:
- Rebate protection: Automatic refunds when insurers underspend on medical care
- Premium transparency: Clear disclosure of how premium dollars are allocated
- Quality incentives: Encouragement for insurers to invest in care improvement
- Profit limitations: Caps on excessive administrative spending and executive compensation
WARNING Insurers may attempt to reclassify administrative expenses as medical costs to meet MLR requirements, making independent verification through state regulatory reports essential for consumers.
State insurance commissioners monitor MLR compliance through annual filings, with health insurance regulations available for public review. Non-compliant insurers face penalties, rebate requirements, and potential market restrictions.
The rule strengthens consumer protection by creating financial incentives for insurers to control administrative bloat while maintaining adequate medical spending. Consumers can request MLR information from insurers during plan selection to identify companies consistently exceeding minimum requirements.
What is a good loss ratio for health insurance?
A good loss ratio for health insurance typically ranges from 80% to 90%, representing the percentage of premium revenue paid out in medical claims, with ratios in this range indicating balanced financial health and adequate member benefits.
The loss ratio differs from the MLR by focusing specifically on claims payments rather than broader medical spending categories. This metric helps consumers evaluate insurer financial stability and claim-paying ability during high-cost medical events.
Loss ratio interpretation guide:
| Loss Ratio Range | Financial Interpretation | Consumer Implications |
|---|---|---|
| 85-90% | Optimal balance | Strong benefits, stable finances |
| 80-84% | Conservative spending | Lower benefits, higher reserves |
| 75-79% | Profit-focused | Potential underutilization |
| Above 90% | High claims activity | Possible premium increases |
Factors affecting health insurance loss ratios:
- Population demographics: Age, chronic disease prevalence, geographic health trends
- Benefit design: Deductibles, copayments, coverage comprehensiveness
- Network management: Provider costs, utilization controls, care coordination
- Underwriting practices: Risk assessment accuracy, premium pricing strategies
- Economic conditions: Healthcare inflation, regulatory changes, market competition
State regulatory authorities analyze loss ratios through federal insurance oversight programs to identify insurers with unsustainable claims patterns. Consistently high ratios may trigger premium rate reviews, while unusually low ratios could indicate inadequate benefits or access barriers.
PRO TIP Target insurers with loss ratios between 82-88% for optimal balance of comprehensive benefits and long-term financial stability, avoiding companies with extreme ratios in either direction.
Consumer considerations for loss ratio evaluation:
- Claims accessibility: Higher ratios may indicate easier claim approval processes
- Premium stability: Moderate ratios suggest predictable premium pricing
- Network adequacy: Balanced ratios support robust provider networks
- Financial strength: Stable ratios indicate sustainable business operations
Regional variations in loss ratios reflect local healthcare costs, with Department of Health and Human Services data showing significant differences between markets. Urban areas typically show higher ratios due to increased healthcare utilization and provider costs.
Investors and rating agencies monitor loss ratios alongside other financial metrics to assess insurer creditworthiness and market competitiveness. Consumers benefit from understanding these patterns when selecting coverage for predictable healthcare needs.
What is the 85% MLR rule?
The 85% MLR rule applies specifically to large group health insurance plans, requiring insurers to spend at least 85% of premium revenue on medical care and quality improvement activities, with stricter standards than the 80% requirement for individual and small group markets.
This enhanced threshold recognizes that large employers possess greater negotiating power and administrative efficiency, enabling insurers to achieve higher medical spending ratios while maintaining profitable operations and competitive pricing.
Large group MLR requirements:
- Minimum medical spending: 85% of premium revenue
- Maximum administrative costs: 15% of premium revenue
- Rebate obligations: Required when falling below 85% threshold
- Quality improvement: Included in medical spending calculation
- Reporting frequency: Annual MLR filings with federal regulators
| Plan Category | Group Size | MLR Threshold | Administrative Limit |
|---|---|---|---|
| Large Group | 101+ employees | 85% | 15% |
| Small Group | 2-100 employees | 80% | 20% |
| Individual | Self-purchased | 80% | 20% |
The Department of Labor demonstrates that most large group plans exceed the 85% requirement, with average MLRs ranging from 87% to 92% across different market segments.
Why large groups face stricter MLR requirements:
- Administrative efficiency: Larger risk pools reduce per-member processing costs
- Negotiating leverage: Employers can demand better pricing and terms
- Simplified enrollment: Reduced marketing and acquisition expenses
- Predictable utilization: Larger populations provide more stable claims patterns
- Competitive markets: Multiple insurer options drive down administrative margins
Benefits for large group members:
- Enhanced value: Higher percentage of premiums spent on actual healthcare
- Lower administrative fees: Reduced overhead costs passed to members
- Improved benefits: More premium dollars available for coverage enhancements
- Greater transparency: Detailed MLR reporting requirements increase accountability
IMPORTANT NOTE Large group plans failing to meet the 85% MLR threshold must distribute rebates to plan participants, with rebate calculations based on the previous three-year average performance.
Self-insured large employers may adopt similar MLR standards for administrative service contracts, even though they’re not subject to federal MLR requirements. These voluntary standards help control third-party administrator costs and ensure efficient claims processing, similar to approaches used in business insurance where companies self-insure certain risks.
Consumer action steps for large group participants:
- Request MLR data: Ask HR departments for plan-specific MLR performance
- Compare options: Evaluate MLR compliance during open enrollment periods
- Monitor rebates: Track any MLR-related rebates distributed to participants
- Advocate improvements: Work with employee committees to demand transparency
State insurance departments provide ACA compliance information showing large group performance relative to small group and individual markets, helping employers make informed coverage decisions.
How do health insurance payout ratios affect consumers?
Health insurance payout ratios directly impact consumers through premium pricing, benefit accessibility, network adequacy, and long-term coverage stability, with higher ratios generally correlating to better value and member satisfaction across multiple dimensions of healthcare access.
When insurers maintain appropriate payout ratios, consumers benefit from predictable premium increases, comprehensive provider networks, and streamlined claims processing that reduces financial barriers to necessary medical care.
Direct consumer impacts of payout ratios:
Premium Stability and Pricing:
- High ratios (85-90%): Sustainable premium growth, value-focused pricing
- Low ratios (below 80%): Potential for excessive premium increases or benefit reductions
- Volatile ratios: Unpredictable premium changes, budget planning difficulties
Claims Processing and Access:
- Balanced ratios: Efficient approval processes, minimal administrative delays
- Unbalanced ratios: Potential for increased denials or processing bottlenecks
- Transparent ratios: Clear communication about coverage decisions and appeals
| Payout Ratio Impact | Consumer Experience | Financial Consequences |
|---|---|---|
| Optimal (85-88%) | Smooth claims, stable premiums | Predictable healthcare budgets |
| Low (below 82%) | Potential access barriers | Higher out-of-pocket risks |
| High (above 92%) | Excellent benefits | Possible premium volatility |
Network adequacy directly correlates with payout ratios through provider reimbursement levels and contract negotiations. Insurers with balanced ratios typically maintain robust networks by offering competitive payment rates to healthcare providers, ensuring members have adequate access to specialists and facilities.
Consumer protection mechanisms tied to payout ratios:
- MLR rebates: Automatic refunds when insurers underspend on medical care
- State oversight: Regulatory monitoring of ratio trends and consumer complaints
- Transparency requirements: Public reporting of financial performance metrics
- Market competition: Pressure for insurers to optimize ratio performance
The Health and Human Services consumer protection shows strong correlation between healthy payout ratios and reduced consumer grievances about claim denials, network access, and customer service quality.
Long-term implications for consumer choice:
- Plan sustainability: Appropriate ratios support stable coverage options
- Innovation investment: Balanced finances enable technology and care improvements
- Market competitiveness: Healthy ratios attract quality providers and retain members
- Regulatory compliance: Consistent ratio performance reduces regulatory intervention risk
PRO TIP Monitor your insurer’s payout ratio trends over 3-5 years to identify patterns that might affect future premium costs, benefit changes, or network stability before making coverage decisions.
Consumers can access payout ratio information through state insurance department websites, annual MLR reports, and insurer financial disclosures. Understanding these metrics empowers informed decision-making during open enrollment periods and helps identify potential coverage issues before they impact care access, much like evaluating home insurance coverage components before purchasing property protection.
Regional market analysis shows that areas with multiple insurers maintaining healthy payout ratios typically offer more competitive pricing and comprehensive benefits, highlighting the importance of market competition in driving consumer value.
What factors influence health insurance payout ratios?
Multiple interconnected factors influence health insurance payout ratios, including population demographics, regulatory requirements, market competition, healthcare cost trends, and operational efficiency, with successful insurers balancing these elements to maintain sustainable ratios while providing quality coverage.
Understanding these factors helps consumers evaluate insurer performance and predict future coverage stability, particularly during periods of healthcare market volatility or regulatory change.
Primary factors affecting payout ratios:
Population and Risk Factors:
- Age demographics: Older populations drive higher medical utilization and claims costs
- Chronic disease prevalence: Diabetes, heart disease, and cancer significantly impact ratios
- Geographic health trends: Regional disease patterns and lifestyle factors
- Employment sectors: Different industries present varying health risk profiles
- Socioeconomic factors: Income levels affect preventive care access and health outcomes
Regulatory and Compliance Requirements:
- MLR mandates: Federal requirements for minimum medical spending
- State benefit mandates: Required coverage for specific services or conditions
- Quality improvement requirements: Mandatory spending on care coordination and outcomes
- Network adequacy standards: Minimum provider access requirements affecting costs
- Prior authorization regulations: State rules governing utilization management
| Factor Category | Impact on Ratios | Insurer Response |
|---|---|---|
| Demographics | High chronic disease = higher ratios | Risk-based pricing, wellness programs |
| Regulations | MLR requirements = minimum ratios | Operational efficiency improvements |
| Market Competition | Competitive markets = optimized ratios | Value-based benefit design |
| Healthcare Costs | Medical inflation = ratio pressure | Provider contract negotiations |
Operational and Strategic Factors:
- Claims processing efficiency: Technology investments reduce administrative costs
- Provider network management: Strategic contracting controls medical expense trends
- Utilization management: Prior authorization and care coordination programs
- Fraud prevention: Detection systems reduce inappropriate claims payments
- Care management: Chronic disease programs improve outcomes and control costs
Market and Economic Influences:
- Healthcare provider consolidation: Hospital mergers increase negotiated rates
- Pharmaceutical costs: Specialty drug pricing significantly impacts medical ratios
- Technology adoption: Digital health tools affect utilization patterns and costs
- Economic conditions: Unemployment impacts enrollment and utilization patterns
- Competitive dynamics: Market concentration affects pricing power and efficiency
The Centers for Medicare & Medicaid Services demonstrate significant regional variation in factors affecting payout ratios, with state-specific healthcare costs and regulatory environments creating distinct market conditions.
Consumer implications of factor analysis:
- Plan selection: Understanding local factors helps predict plan stability
- Cost forecasting: Regional trends inform premium increase expectations
- Network evaluation: Market factors affect provider availability and access
- Long-term planning: Demographic trends influence future coverage needs
IMPORTANT NOTE Insurers operating in multiple states may show different payout ratios by market due to varying regulatory requirements, provider costs, and population health characteristics.
Strategic responses by insurers to manage ratio factors:
- Vertical integration: Owning provider networks to control costs and quality
- Population health initiatives: Preventive care programs reducing long-term costs
- Data analytics: Predictive modeling for risk assessment and intervention
- Value-based contracts: Provider payment models tied to quality and outcomes
- Digital transformation: Technology solutions improving operational efficiency
State insurance departments monitor these factors through federal regulatory compliance to ensure insurers maintain appropriate ratios without compromising consumer access or quality of care.
FAQ
How often do health insurance companies report payout ratios?
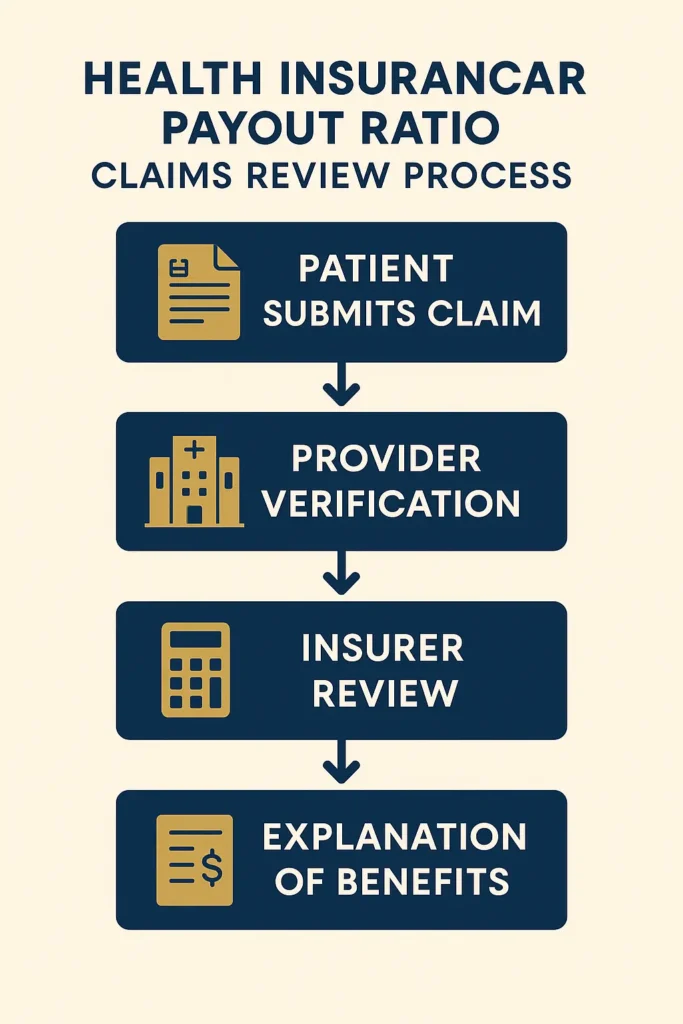
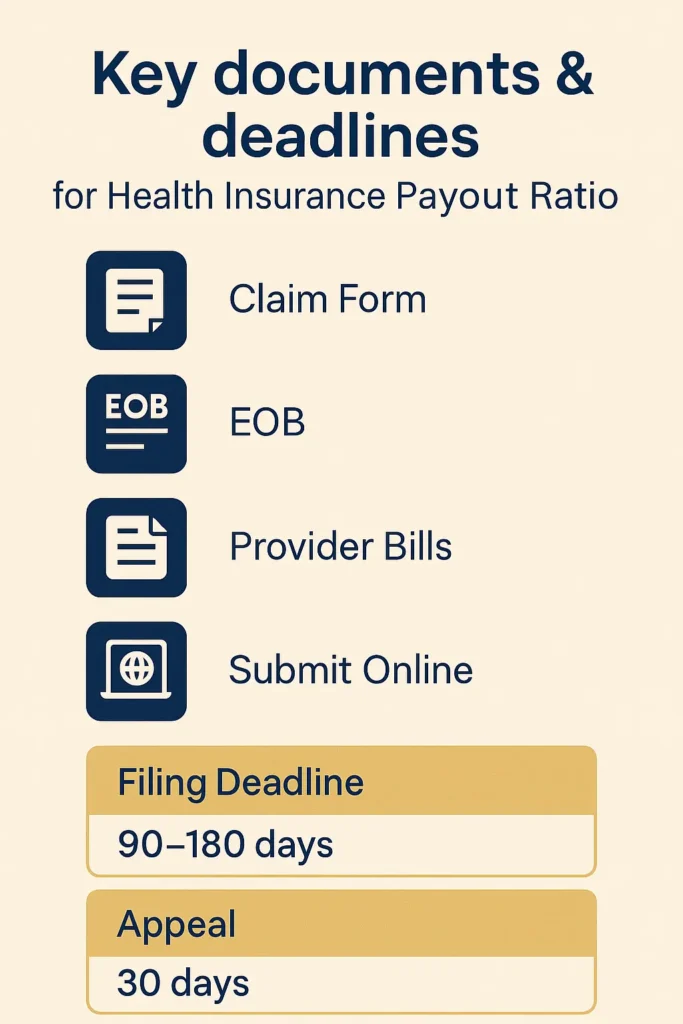
Health insurance companies report payout ratios annually through MLR filings submitted to federal and state regulators by June 1st each year, with data covering the previous calendar year’s financial performance and claims activity.
The Medical Loss Ratio (MLR) reporting process requires detailed documentation of premium revenue, medical expenses, quality improvement costs, and administrative expenditures. State insurance departments make these reports publicly available, typically within 60-90 days of submission.
Can consumers access individual insurer payout ratio data?
Yes, consumers can access insurer-specific payout ratio information through multiple sources, including state insurance department websites, the National Association of Insurance Commissioners database, and annual MLR summary reports published by the Centers for Medicare & Medicaid Services.
Most state insurance departments provide searchable databases allowing consumers to compare MLR performance by insurer, market segment, and geographic region. This transparency helps consumers make informed coverage decisions during open enrollment periods.
What happens if an insurer’s payout ratio is too low?
Insurers with payout ratios below MLR requirements must issue rebates to policyholders, calculated as the difference between required and actual medical spending ratios applied to total premium revenue for the relevant period.
Rebates are distributed annually, typically between July and September, either as direct payments to consumers or premium credits for the following year. Large group plans distribute rebates to plan participants through employers, while individual market rebates go directly to policyholders.
Do payout ratios vary by insurance plan type?
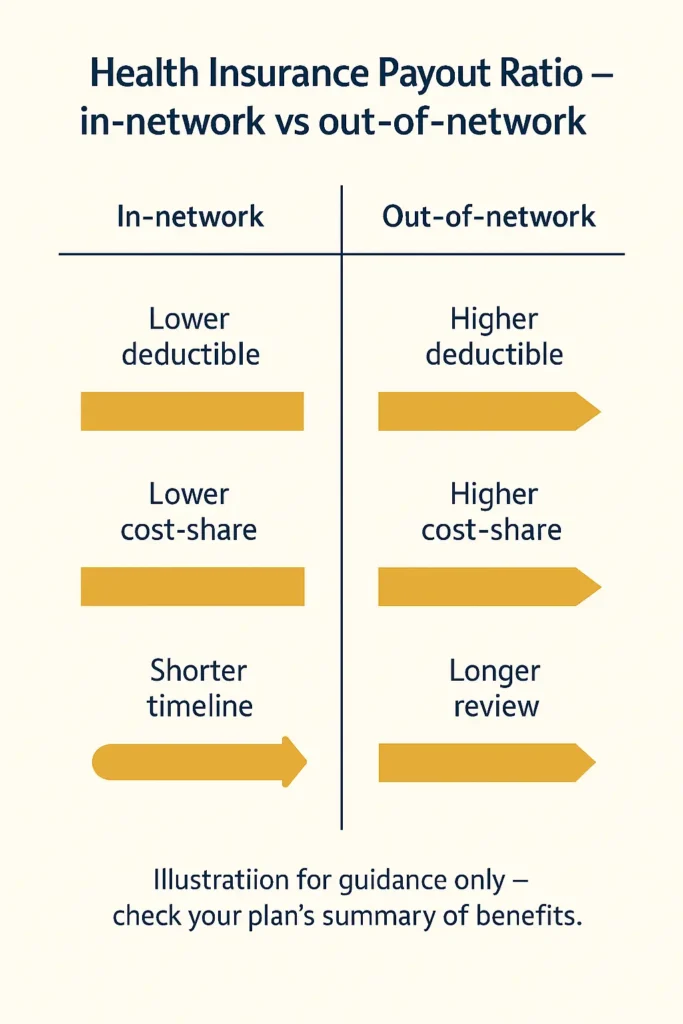
Payout ratios vary significantly by plan type and market segment, with Health Maintenance Organization (HMO) plans typically showing higher ratios than Preferred Provider Organization (PPO) plans due to different cost management approaches and utilization patterns.
High-deductible health plans often demonstrate lower initial ratios but may exceed traditional plan ratios once deductibles are met. Short-term and supplemental insurance products are exempt from MLR requirements and may show substantially different payout patterns.
How do health insurance payout ratios compare internationally?
U.S. health insurance payout ratios are generally lower than those in countries with single-payer systems, where administrative costs typically represent 2-8% of total healthcare spending compared to 15-20% allowed under U.S. MLR requirements.
International comparison data from the OECD shows that countries with universal healthcare systems achieve higher effective payout ratios through reduced administrative complexity and standardized claims processing.
Can payout ratios predict future premium increases?
Payout ratios provide valuable insight into potential premium changes but must be analyzed alongside healthcare cost trends, regulatory changes, and market competition to accurately predict future pricing.
Insurers with consistently high ratios may face pressure for premium increases to maintain financial stability, while those with low ratios may have more flexibility to absorb cost increases without passing them to consumers. Three-year ratio trends offer better predictive value than single-year data.
Conclusion
Health insurance payout ratios serve as critical indicators of insurer financial health, consumer value, and market competitiveness in the evolving healthcare landscape. Understanding these metrics empowers consumers to make informed health insurance coverage decisions while providing transparency into how premium dollars translate into actual healthcare benefits.
The federal MLR requirements of 80% for individual and small group markets and 85% for large group plans establish minimum standards for medical spending, with rebate mechanisms protecting consumers from excessive administrative costs. However, optimal ratios typically exceed these minimums, ranging from 85-90% for sustainable operations that balance member benefits with long-term stability.
Key consumer takeaways for using payout ratio information:
- Research insurer MLR performance over multiple years before selecting coverage
- Understand how regional factors and demographics influence local market ratios
- Monitor annual rebate notifications as indicators of insurer compliance and value
- Evaluate payout ratios alongside other quality metrics like claim settlement rates and network adequacy
As healthcare costs continue rising and regulatory frameworks evolve, payout ratios will remain essential tools for assessing insurer performance and protecting consumer interests in an increasingly complex insurance marketplace.
Key Takeaways
- Health insurance payout ratios measure the percentage of premium revenue spent on medical care, with federal MLR requirements establishing minimum thresholds of 80-85% depending on market segment
- Optimal payout ratios typically range from 85-90%, balancing comprehensive member benefits with sustainable insurer operations and predictable premium pricing
- Consumers can access payout ratio data through state insurance departments and federal reporting systems, enabling informed comparison of insurer performance during coverage selection
- Multiple factors influence payout ratios, including population demographics, regulatory requirements, healthcare cost trends, and operational efficiency measures
- Ratios below MLR thresholds trigger automatic rebates to consumers, providing financial protection against excessive administrative spending by insurance companies
Disclaimer
Data freshness: Insurance rates and regulations change frequently. Data accuracy depends on timing of official releases.
Geographic variations: Insurance requirements vary significantly by state. Always consult your state’s insurance department.
Professional advice: This information is for educational purposes only. Insurance decisions should be made in consultation with licensed professionals.